INTRODUCTION
Lateral epicondylitis, commonly known as tennis elbow, is characterised by pain at the muscle attachments on the lateral epicondyle. Pain generally increases with local pressure, with active extension of the wrist, or through stretching of these muscles. Lateral epicondylitis is one of the most common lesions of the elbow, affecting 1–3% of the population.1 ,2 The symptoms generally have an insidious onset or, more rarely, are associated with acute symptoms accompanying a traumatic process.3 ,4 The average duration of a typical episode ranges from 6 to 24 months, with most patients reporting recovery by 52 weeks.5 In some cases, symptoms do not resolve and lead to chronic disease (between 5% and 10%), with these patients eventually undergoing surgery.6 ,7
Lateral epicondylitis has traditionally been defined and treated as an inflammatory process.8 From this perspective, different methods have been used in an attempt to treat the condition, such as corticosteroid injections or various physiotherapy modalities.9 However, several studies have shown that the short-term symptomatic benefits obtained using these methods decline over time, leading to high lateral epicondylitis recurrence rates in the mid to long term.10–12 Furthermore, in these studies the actual effect that these techniques have on the tissue is uncertain, as the structural changes seen on ultrasound (US) examination prior to treatment are still present in the majority of patients after treatment.
At present, the prevailing opinion is that lateral epicondylitis is a degenerative or failed healing response within the tendon.13–16 Histological studies have shown degenerative changes without signs of traditional inflammation17 and the presence of proinflammatory agents (eg, neuropeptides, prostaglandins, cytokines and various growth factors).18 Studies using MRI, US and Doppler have also shown degenerative structural tendon changes and hypervascularity, most commonly affecting the extensor carpi radialis brevis (ECRB).19 ,20 With this renewed understanding there is increased interest in providing treatments aimed at the regeneration of tissues with poor healing potential (eg, platelet-rich plasma (PRP),21 radiofrequency,22 percutaneous needle tenotomy (PNT),23 ,24 dry needling,25 ,26 acupuncture27 or percutaneous needle electrolysis (PNE)28).
US-guided PNE is a novel minimally invasive approach which involves the application of a galvanic current through an acupuncture needle. PNE is a combination of mechanical and electrical stimulation as a method to provide a controlled microtrauma to the affected soft tissue structures. The needle is directed into the soft tissue lesions under direct visualisation using the US machine. The technique stimulates a local inflammatory response in which there is increased cellular activity and repair of the affected area.28–30 PNE has proved to be effective in the short term (6 weeks from baseline) in patellar tendinosis,28 but its effectiveness in chronic lateral epicondylitis is still unknown.
The purpose of this study was to evaluate the clinical and ultrasonographic effectiveness of a multimodal programme in patients with chronic lateral epicondylitis using US-guided PNE and exercises in the short term, and to evaluate whether the clinical outcomes in such patients decline over time (at 26 and 52 weeks follow-up).
METHODS
Design and participants
We performed a one-way repeated measures study over time. Measures were obtained pre-intervention, at treatment discharge and at 6, 26 and 52 weeks follow-up.
Consecutive patients from a clinical setting in Spain were considered eligible if they met the following inclusion criteria: (1) pain over the lateral humeral epicondyle provoked by at least two of the following: gripping, palpation, stretching of forearm extensor muscles and resisted wrist or middle finger extension; (2) persistent pain for at least 3 months despite conservative treatments including medication (oral non-steroidal anti-inflammatory drugs and analgesics), brace application or physiotherapy; (3) age 18–45 years; and (4) structural tendon changes at the origin of the extensors, demonstrated during musculoskeletal US. Exclusion criteria were: (1) patients with a history of advanced cervical arthrosis in the C4–C6 segments; (2) bilateral lateral epicondylitis with central sensitisation; (3) symptoms compatible with posterior interosseous nerve entrapment; (4) previous surgery, fractures, trauma or a previous history of rheumatic disorders in the area of the lateral epicondyle; (5) history of corticosteroid injection at the lateral epicondyle within the last 3 months. Two experienced professionals performed recruitment and examination of subjects in order to assess for eligibility criteria. All eligible patients provided written informed consent.
Intervention
Patients received one session of PNE per week over 4 weeks (or over 6 weeks when pain persisted) associated with a home programme consisting of eccentric exercise (EccEx) and stretching, initiated 24 h after each session. The EccEx and stretching programme was taught by a physiotherapist in the first session and monitored in subsequent sessions. At discharge, patients were instructed to perform only EccEx once daily for the first 6 weeks of the follow-up period.
PNE was performed under US guidance on the clinically relevant area (or areas of maximum tenderness to palpation and with ultrasonographic degenerative tendon changes) using an intensity of 4–6 mA during 3 s, approximately three times (figure 1A–D). The electrotherapy equipment used (Cesmar Electromedicina, Barcelona, Spain) produces a continuous galvanic current through the cathode (modified electrosurgical scalpel with the needle) while the patient holds the anode (handheld electrode) (figure 2). The ultrasound machine was a GE Logiq E Portable Ultrasound Machine with GE Linear probe 12L-RS (5–13 mHz) (GE Healthcare, Wisconsin, USA). During PNE the patient was placed in a supine position with the affected elbow placed in a position of 90° flexion and pronation. The elbow was sterilised and the sonographic transducer, enclosed in a sterile cover over sterile applied gel, was placed at the lateral epicondyle (first approach) and over the humeroradial joint between the head of the radius and the capitulum of the humerus (second approach),29 where it remained throughout the procedure. A common target area was the deep surface of the common extensor tendon (origin of the ECRB and the extensor digitorum communis) (first approach) and the deep surface of the ECRB, over the capsule and the lateral ulnar collateral ligament (second approach). A 0.3×25 mm (1 inch) acupuncture needle (Cloud & Dragon; uncoated steel needle with rigid metal handle without guide, Japanese type) was inserted at a 30–45° angle to the skin in the direction of the lateral epicondyle (first approach) (figure 3A) and at a 80° angle to the skin with the needle tip directed towards the humeroradial joint (second approach) (figure 3B). In the first approach the needle was advanced parallel to the longitudinal plane of the tendon (in-plane approach) whereas, in the second approach, the needle was advanced along the short plane of the humeroradial joint (out-of-plane approach). Real-time ultrasonographic imaging provided guidance for both procedures.29 Once the needle reached the target tissue, readjustments of the needle position were made in order to ensure correct stimulation (see online supplementary video 1). The generation of the galvanic current (the cathodic flow is usable with fixed polarity) creates a white image (hyperechoic) as a result of the liberation of hydrogen gas due to the electrolysis (see online supplementary video 2). Oral paracetamol was used when necessary for the purpose of pain relief only.
Figure 1
(A) Long-axis grey-scale ultrasound image displaying the origin of the extensor tendon during needle placement showing the echogenic needle (arrowheads) with the distal tip in the area of tendinosis. (B–D) Percutaneous needle electrolysis was performed with continual sonographic guidance. A white area is observed in the tissue approximately 30 min post-intervention. LE, lateral epicondyle.
Figure 2
Detail of cathode (modified electrosurgical scalpel with the needle) and anode (handheld electrode) electrodes for percutaneous needle electrolysis.
Figure 3
Needle approach. (A) In-plane approach. The transducer is placed on the lateral epicondyle and the needle is inserted in the centre of the transducer in a long axis position at an angle of about 30–45° to the skin surface, depending on the target area, and then advanced parallel to the sound beam. (B) Out-of-plane approach. The transducer is placed over the humeroradial joint and the needle is positioned at the centre of the transducer in a short axis position at an angle of about 80° to the skin surface and advanced perpendicular to the sound beam. LE, lateral epicondyle; RH, radial head; yellow line, lateral ulnar collateral ligament; blue line, capsule of the humeroradial joint; pink structure, common extensor tendon.
The EccEx programme consisted of three series of up to 10 repetitions of eccentric work, repeated twice daily (morning and afternoon) under maximum load (initially with 1 kg) in an optimal and functional pain-free range. From maximum wrist extension and radial deviation, rapid wrist flexion movements were performed followed by a 2 s hold of the final position. In between series patients were given a rest period of 2–3 min. This formula was used for the duration of the physiotherapy programme. The concentric contraction phase for returning to the starting position was nullified with the help of the other hand.31 ,32
The stretching programme consisted of a stretching exercise for the epicondylar muscles consisting of three series of seven repetitions twice a day (morning and afternoon), performed in a sitting position with a flexed wrist and fingers, ulnar deviation and elbow extension reaching the stretch limit without bounces, and held for 45 s, with a 30 s rest between repetitions.33 ,34
OUTCOME MEASURES
Outcome measures throughout the treatment and during the short-term follow-up period (6 weeks) were severity of pain (rating of pain intensity, pain-free pressure and provocation tests), disability and structural tendon changes.
Intensity of elbow pain during activity was recorded using a visual analogue scale score (0=no pain; 100=maximum intensity), pain-free pressure was measured with a digital algometer (Wenzhou Sundoo Instruments, China) and Cozen and Thompson tests were performed in order to provoke localised pain over the lateral epicondyle. Disability was measured with the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire (0–100 where 100 is the higher disability).35 Structural tendon changes were examined in the lateral epicondylar area, including the origin of the extensor tendon, ECRB and the adjacent soft tissues with a GE Logiq E Portable Ultrasound Machine under the guidelines defined by the European Society of Musculoskeletal Radiology.36 Structural tendon changes (tendon thickening, hypoechogenicity and intrasubstance tears) were demonstrated by the grey scale US, and hypervascularity (not present or several areas) by Power Doppler examination. The same experienced professional performed all US and Power Doppler examinations and was blinded to the treatment.
At the 6 week follow-up we calculated recurrence rates as an increase in severity of pain or disability compared with the measures at discharge. We also measured patients’ perceptions of the overall outcome using a 4-point scale where ‘excellent’ represented full return to all activity with no pain, ‘good’ represented full return to all activity with occasional mild pain, ‘fair’ represented no pain present with normal activities but significant pain with heavy activities and ‘poor’ represented little or no relief of preoperative symptoms. Success rates were then calculated based on the perception of overall outcome; we considered excellent or good to be ‘successful’ and fair or poor to ‘unsuccessful’.10
Outcome measures throughout the mid- and long-term follow-up period (26 and 52 weeks) were the perception of overall outcome and success rates, as measured at 6 weeks, and the recurrence rates beyond 6 weeks, as the number of cases that went from ‘successful’ at 6 weeks to ‘unsuccessful’ on overall outcome at 26 or 52 weeks.
STATISTICAL ANALYSIS
Data entering, management and analysis were performed with SPSS V.15.0 software for Windows (SPSS, Chicago, Illinois, USA) and a value of p<0.05 was chosen as the level of statistical significance. The absolute and relative frequencies and the descriptors of the main variables of the study were quantified. Paired Student t tests and χ2 tests were used to statistically evaluate changes in the parameters.
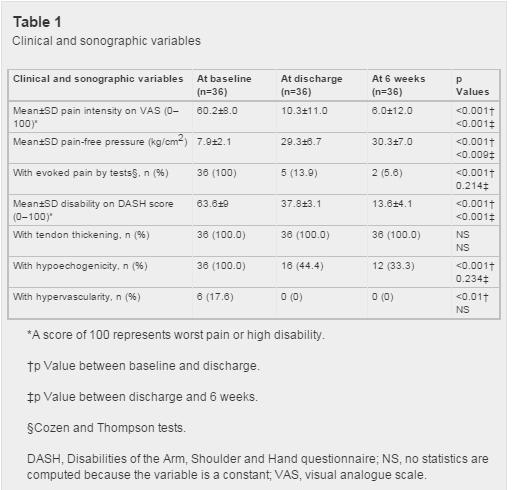
RESULTS
A total of 36 consecutive patients were included in the study (52.8% men) with a mean (SD) age of 38 (6.4) years; 88.9% performed manual work with repeated movements and forceful activities affecting the epicondylar muscles (eg, officials, plumbers, waiters or firemen) and 75% practised sports with manual mechanical loading (eg, paddle tennis). The duration of symptoms ranged from 6 to 20 months (mean (SD) 12.6 (4.1) months). Table 1 shows patients’ clinical and structural characteristics at baseline. The mean score of both pain intensity and disability measurements were higher than 60. All patients had evoked pain, as measured by orthopaedic tests as well as hypoechogenicity and tendon thickening, and only six presented with hypervascularity.
None of the patients discontinued treatment during the study period. No complications or adverse events appeared during or after the intervention.
All patients participated in the 6-week follow-up, but only 32 (88.8%) were interviewed at 26 and 52 weeks. Of those lost to follow-up, all dropped out because they could not be located. Those lost to follow-up did not differ from participants with respect to demographic background or baseline pain and disability scores.
OUTCOMES AT DISCHARGE
Table 1 shows the outcome data. We found significant differences in all outcome measures between pre-intervention and discharge. Ratings of pain intensity, pain-free pressure and disability changed more than 40, 20 and 25 points in their respective scores. Pain by provocation decreased in 31 patients (86.1%) whereas hypoechogenicity values decreased in 20 patients (55.5%) and hypervascularity decreased in all six cases (100%) (figure 4A–D). There were no statistically significant differences among the group of patients that improved at 4 or 6 weeks.
Figure 4
Lateral epicondylitis in a patient with a history of chronic right lateral elbow pain. (A) At baseline, long-axis grey-scale ultrasound (US) image reveals an irregular structure and a hypoechoic focus (asterisks) in the deep fibres of the extensor carpi radialis brevis. (B) At 6 weeks follow-up, US image of the same patient shows structural changes inside the initial area (arrowheads). (C) Power Doppler imaging demonstrates a striking hypervascular pattern composed of a series of tiny vessels. (D) Power Doppler imaging shows no blood flow inside the initial area. LE, lateral epicondyle; RH, radial head.
OUTCOMES AND RECURRENCES DURING FOLLOW-UP PERIOD
At 6 weeks we also found significant differences compared with discharge for almost all outcome measures (table 1). No significant differences was found at 6 weeks compared with discharge for evoked pain and hypoechogenicity values as the measures used left little room for improvement after discharge.
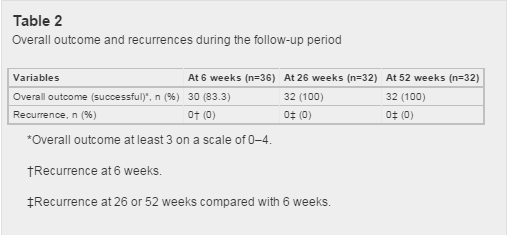
Table 2 shows that most patients (30, 83.3%) rated the overall outcome as ‘successful’ at 6 weeks. The six remaining patients categorised as ‘unsuccessful’ received a final session of PNE to deal with a localised point of residual pain. At 26 and 52 weeks all participants in this follow-up period (n=32) perceived a ‘successful’ outcome.
After discharge no patients demonstrated deteriorated pain or disability scores at 6 weeks and therefore recurrences were 0%. Recurrence rates after 6 weeks were also null in the mid to long term.
DISCUSSION
In this study a multimodal programme of PNE and exercises was associated with a reduction of pain severity, disability and degenerative structural changes at discharge and in the short-term (6 weeks) follow-up period. This programme also showed that clinical and ultrasonographic benefits at discharge did not decline in the short term, and that no recurrences in the mid to long term were reported on the overall outcome achieved at short term.
Our study supports the current theoretical model of tendinopathy as a degenerative process.15 ,19 An interesting finding was that hypoechogenicity and tendon thickening was more frequent than hypervascularity. The hypervascular area found in the origin of the extensor seems to be related to pain,16 however more studies are needed to clarify this suggestion as there are patients with pain but without blood flow. Also, in this study the hypoechoic regions were most frequently found in the deep fascicle of the ECRB at its insertion and over the humeroradial joint, a finding concurrent with other studies.19 ,20
Moreover, our study supports evidence that, both at discharge and in the short term, many patients experience a reduction in the degenerative structural changes (hypervascularity and hypoechogenicity) seen at baseline on US examination. A reduction in hypervascularity has been found with other therapies,12 but after longer periods of follow-up. The biological basis for the structural effect of PNE is still largely unknown; the early response may be due to both the mechanical and biochemical effects of PNE which provoke tenocyte disruption, as well as local inflammatory processes occurring in the soft tissue which enable phagocytosis and repair of the affected tissue.27–30 The hypoechoic regions and the area of hypervascularisation are small and localised in chronic lateral epicondylitis, circumstances that could facilitate the elimination or significant short-term reduction in a few sessions. Our opinion is that changes in the structure of the tendon (tendon thickening) would take longer because they require a biomechanical process of remodelling and maturation.
A review of the current literature has shown that corticosteroid injections can be useful for improving symptoms in the short term (generally 2–6 weeks).9 ,11 ,37 However, for the assessment of long-term benefits (generally >6 months), most randomised trials do not show any benefit for treatment with steroids over placebo injection, physiotherapy or rest alone.9 ,11 ,37 All these techniques achieve a greater or lower level of pain reduction and improvement in function, but they fail to repair the tendon as they fail to successfully remodel the structure38 or exacerbate the tissue in order to achieve a new proliferation.39 ,40 In our opinion, and considering our results, the current theoretical model of tendinopathy as a degenerative process mainly associated with a failure in the process of tendon repair requires different and new therapeutic approaches. If this is not a reactive inflammatory process, why perform anti-inflammatory treatments? What is the real effect obtained from these treatments, and what progression should they follow?
The progress of patients seen at discharge and in the short term was not solely due to PNE and the natural history of the condition, but also to the EccEx and muscle stretching performed at home. In our opinion, PNE stimulates the tendon’s biology and causes the initial inflammatory response in the repair phase,27–30 while early controlled mechanical loading (EccEx and stretching) facilitates the process of collagen tissue proliferation, thus improving the biomechanical properties of the stimulated tendon. In this regard, Virchenko and Aspenberg41 studied the effect of PRP on the Achilles tendon of rats subjected to subsequent loading or unloading and found that, after 14 days, the PRP effects in the unloading group disappeared and the mechanical properties of the stimulated tissue were reduced to less than half compared with normal tissue. Moreover, the type of exercise (mechanical loading) can play a crucial role, as evidence shows that eccentric training seems to be the best option for these patients.31 ,32 ,42 Alongside these factors, if we rely on clinical experience, in chronic lateral epicondylitis cases the isolated application of EccEx and stretching is insufficient to obtain an optimal functional outcome.43 Finally, along the same lines as the proposed programme (PNE+EccEx+stretching), other authors are including a combination of other interventions in lateral epicondylitis (eg, PRP, PNT), together with eccentric training programmes and stretching with similar characteristics, in order to promote positive therapeutic results.24 ,44
A major finding of our study was that the clinical outcomes achieved with this treatment programme did not decline over time. A common problem occurring in the usual treatments for chronic lateral epicondylitis in the mid to long term are the high recurrence rates which vary between 34% and 72%.8 ,9 In these cases, patients often improve with conventional physiotherapy programmes usually associated with rest from sports and the use of a counterforce brace,45 but when they return to sport or perform activities of equal or greater intensity, symptoms are often present. Our study found no recurrence in the patient sample despite the fact that 75% of the patients performed some form of sports activity.
This study has a number of limitations, mainly due to the absence of a control group in order to compare the results obtained with placebo or another intervention. However, case series are useful in several situations, including the discovery of novel treatments and the detection of unexpected benefits or risks of a treatment. We have found no similar studies available in the scientific literature, probably due to the fact that this treatment technique has only recently been developed. The findings from this case series should be tested with the use of more rigorous study designs that include a comparison group in double-blind, placebo-controlled, randomised studies with a larger sample.
CONCLUSIONS
Symptoms and degenerative structural changes of chronic lateral epicondylitis are reduced after US-guided PNE associated with EccEx and stretching, with encouragingly low recurrences in the mid to long term.
Artículo cedido por los fisioterapeutas Fermín Valera y Francisco Minaya Profesores del curso Electrólisis Percutánea Musculoesquelética Ecoguiada (EPM) Autores del libro «Fisioterapia Invasiva» Consulta el currículum completo de Fermín Valera en: http://www.instema.net/quienes-somos/profesores/dr-fermin-valera/ Consulta el currículum completo de Francisco Minaya en: http://www.instema.net/quienes-somos/profesores/dr-francisco-minaya/ Curso de Electrólisis Percutánea Musculoesquelética Ecoguiada (EPM): http://www.instema.net/producto/electrolisis-percutanea-musculoesqueletica-ecoguiada-epm/ Link al artículo original: http://aim.bmj.com/content/32/6/446.full
Comments are closed.